Clinical Study
Clinical and biochemical evaluation of home use
of an oral irrigator (SoWash)
in patients affected by gingivitis and periodontitis.
INTRODUCTION
Supra and sub gingival irrigation is considered by clinicians as potentially effective in the elimination of bacterial etiological agents, in both professional and home use. The mechanism of oral irrigation involves the reduction of deposits of bacterial plaque that can lead to periodontal disease (1).
In fact, the primary objective of supragingival irrigation is to wash away the bacteria localised on the dental crown, decreasing the potential for developing gingivitis or decreasing the amount of pre-existing gingival inflammation.
Supragingival irrigation can be considered a valid aid for individuals with poor oral hygiene: the greatest benefits have been found in patients with inadequate interproximal hygiene.
Numerous studies investigating the effect of the oral irrigator on gingivitis and periodontitis have concurred in showing a certain level of efficacy in reducing the inflammation parameters. Cutler et al.(2) showed an effect of the irrigator in modulating the level of proinflammatory cytokines present in the gingival sulcus, thus justifying the efficacy of this type of defence against gingivitis and periodontitis.
Newman et al. 3) showed the irrigator to be effective as an adjunctive treatment to habitual oral hygiene in terms of both the gingival index and the reduction of bleeding on probing, when compared to normal oral hygiene in patients with early onset periodontitis treated in the sphere of periodontal support therapy. In a review of the literature on oral irrigation in 1993, Stein (4) affirmed that adjunctive use of the oral irrigator can play an important role in controlling gingivitis and periodontitis. The positive effect on periodontitis could be attributed in part, as demonstrated by Eakle et al. (5), to the ability of the liquid thrust by the jet to penetrate the periodontal pockets to about 50% of their depth. Cutler et al. (2) showed that the addition of irrigation in diseased interproximal sites produces a significant reduction of the probing depth, the plaque index, and the gingival index with respect to the normal procedures of oral hygiene and the suspension of oral hygiene, also attributing the effect to a mechanism whereby the levels of proinflammatory and anti-inflammatory cytokines in the sulcus are modified.
The oral irrigator has often been recommended as an aid to oral hygiene in orthodontic patients, where the brackets, bands, and arches certainly make home hygiene more complicated (6). In a study on a sample group of orthodontic patients, Burch et al. (7) showed a significant reduction of plaque and bleeding in patients who used the oral irrigator as an adjunct to brushing.
Oral irrigator and clinical parameters
In a study conducted on fifty patients affected by gingivitis and/or periodontitis, we evaluated the clinical efficacy of the use of the SoWash water jet system. The subjects recruited for the study used the SoWash device twice a day for 14 days.
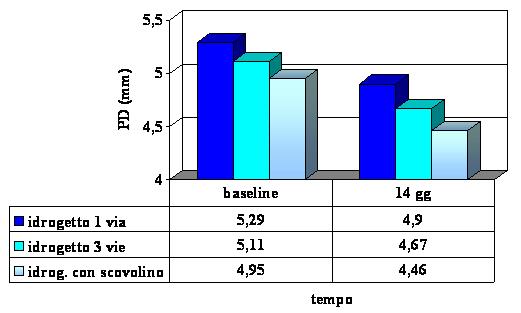
Probing depth (PD)
The reduction of the probing depth was found in all the groups, underscoring an improvement in the clinical conditions of the periodontal pocket.
Bleeding on probing (BOP)
The index of bleeding was reduced during the course of the study in all the groups, to a larger degree in the groups that used the three-way water jet and the water jet with sulcus tip.
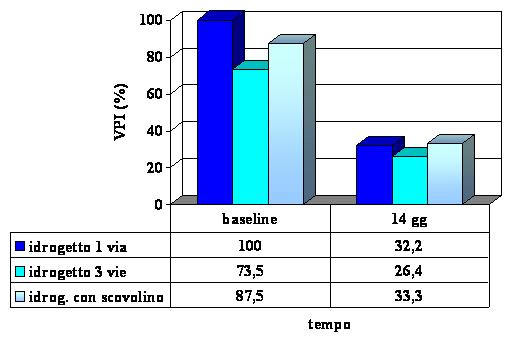
Visible plaque index (VPI)
Oral irrigator and biochemical parameters
To assess the modifications in the biochemical composition of the sulcular fluid, samples of crevicular fluid were taken from the patients recruited for the study in order to make a biochemical determination of the principal markers of inflammation by means of an immunoenzymatic method (ELISA).
In just fourteen days of use, the action of the SoWash device led to a reduction of the total volume of crevicular fluid (GCF) up to 10% in the sites treated with the water jet with sulcus tip. As regards the composition, we monitored the levels of interleukin 1beta (IL-1ß) and metalloproteinase-8 (MMP-8), indicators of inflammation, that were present in the crevicular fluid (GCF).
The efficacy of the treatment should therefore be understood as a reduction of the quantity of these markers in the GCF.
Variation of the composition of the crevicular fluid
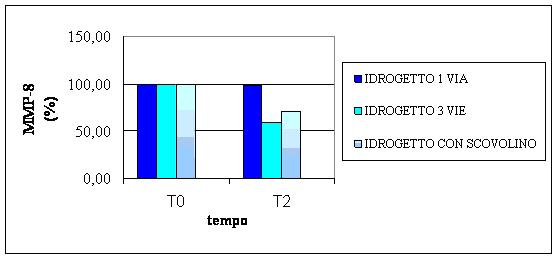
MMP-8
The graph shows the mean values (expressed as a percentage) of the concentration of MMP-8 in the crevicular fluid. The concentration of MMP-8 was reduced by 40% in the sites treated with three-way water jet and by 30% in the patients who used the water jet with sulcus tip.
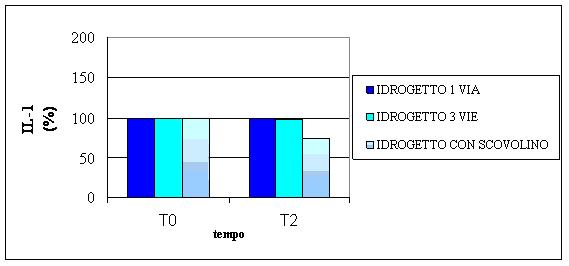
IL-1ß
The graph shows the mean values (expressed as a percentage) of the concentration of IL-1bin the crevicular fluid. IL-1ß showed a substantial reduction in the sites treated with water jet with sulcus tip, corresponding to almost 30% of the initial value.
DISCUSSION
The results of the study show that the use of the SoWash irrigator improves the clinical-biochemical situation following treatment. The mechanism of the system is based on the washing effect of the jet of water and, therefore, on the reduction of the level of bacteria responsible for the activation and propagation of the inflammatory response that destroys tissues. From the clinical point of view, the use of the device demonstrated a strong reduction of the bacterial plaque, in particular with the use of the one-way water jet.
From the biochemical point of view, in our study the SoWash irrigator demonstrated appreciable improvements in terms of the composition of the crevicular fluid. In particular, the water jet with sulcus tip showed the most encouraging results in terms of reduction of IL-1ß and MMP-8 levels, key factors in inflammation and tissue damage. The study also showed a considerable effect of the three-way water jet particularly on the level of MMP-8.
The use of the SoWash water jet with sulcus tip, the only instrument of this type on the market, stimulated interest in its use on the part of the patients with large interproximal spaces, who may or may not have used in the past the traditional type of pick. The mechanical action of the sulcus tip with simultaneous irrigation of the interproximal spaces is a valid aid in cleaning these sites, which are notoriously more difficult to clean.
CONCLUSIONS
The oral irrigation carried out with the SoWash water jet appears to provide results comparable to those obtained in other studies using electric irrigators. The advantage of SoWash device lies in the energy savings, making it more environmentally friendly, and in the portability of the irrigator, which makes it easy to use also when travelling.
In patients with periodontitis and large interproximal spaces, the sulcus tip can be useful with the common indications for using this type of tip, which certainly adds a massage that most of the patients found to be extremely pleasant.
In conclusion, for patients who have difficulty practicing good oral hygiene by brushing alone, for those with orthodontic appliances, and in all cases of difficult cleaning of the interdental spaces, there appears to be a clear advantage in the use of the SoWash water jet system.
BIBLIOGRAPHY
- Greenstein G. The role of supra- and subgingival irrigation in the treatment of periodontal diseases. Position paper: Committee on Research, Science and Therapy, American Academy of Periodontics. Chicago Illinois (1995).
- Cutler CW, Stanford TW, Abraham C, Cederberg RA, Boardman TJ, Ross C. Clinical benefits of oral irrigation for periodontitis are related to reduction of proinflammatory cytokine levels and plaque. J. Clin Periodontol 2000; 27, 134-143.
- Cutler CW, Stanford TW, Abraham C, Cederberg RA, Boardman TJ, Ross C. Clinical benefits of oral irrigation for periodontitis are related to reduction of proinflammatory cytokine levels and plaque. J. Clin Periodontol 2000; 27, 134-143.
- Newman MG, Cattabriga M, Etienne D, Flemmig T, Sanz M, Kornman KS, Doherty F, Moore DJ, Ross C Effectiveness of adjunctive irrigation in early periodontitis:multicenter evaluation J Periodontol 1994 mar;65(3):224-9.
- Stein MA literature review: oral irigation therapy. The adjunctive roles for home and professional use Probe 1993 jan-feb;27(1):18-25
- Eakle WS, Ford C, Boyd RL Depth of penetration in periodontal pockets with oral irrigation J Clin periodontol 1986 Jan;13(1):39-44
- Di Murro C, Paolantonio M, Petti S, Tomassini E, Festa F, Grippaudo C, Sbolgi S The clinical and microbiological evaluation of the efficacy of oral irrigation on the periodontal tissues ofpatients wearing fixed orthodontic appliances Minerva stomatol 1992 nov;41(11):499-506
- Burch JG, Lanese R, Ngan P A two month study of the effects of oral irrigation and automatic toothbrush use in an adult orthodontic population with fixed appliances. Am J Orthod Dentofacial Orthop 1994 Aug;106(2):121-6